Coronary bypass surgery — just what we want to avoid if possible. Daily supplementation with a highly absorbable Q10 dissolved in vegetable oil in a soft-gel capsule could well make a difference.
Heart failure?! Heart failure sounds like it means that the heart has stopped working, right? What is chronic heart failure, exactly, and what are the causes? We know now that supplementation three times a day with 100 mg of a highly absorbable Q10 preparation will have statistically significant (and clinically significant) beneficial effects on patients suffering from chronic heart failure. So what is going on with chronic heart failure patients?
Q10 and lifestyle changes for heart failure patients
A quick look at the Mayo Clinic website tells me that heart failure, sometimes also called congestive heart failure, is the condition of having a heart that is no longer able to pump the blood in the way that a healthy heart would do. The heart muscle has become weakened or stiff or thickened to the extent that it can no longer pump the blood to the body as well as it should. The Mayo Clinic staff members write that many (though not all) patients with heart failure can make lifestyle changes to reverse some of the effects of the condition:
- Exercise if possible
- Lose weight
- Stop smoking and cut back on alcohol
- Reduce exposure to stress
- Eat more fruits and vegetables
- Cut back on the salt (and on the sugar!)
- Take proper care of teeth and gums
To this list, we want to add the taking of a well-absorbed Q10 supplement similar to the one used in the Q-symbio clinical trial enrolling heart failure patients.
Warning signs of possible heart failure
What are the symptoms telling me that I need to have a doctor check my heart? Most of the symptoms are fairly obvious and known to most of us. The Mayo Clinic staff warns about the following warning signs:
- Fatigue and weakness
- Shortness of breath
- Swelling and/or pain in the legs
- Rapid heartbeat or irregular heartbeat
Multiple causes of heart failure
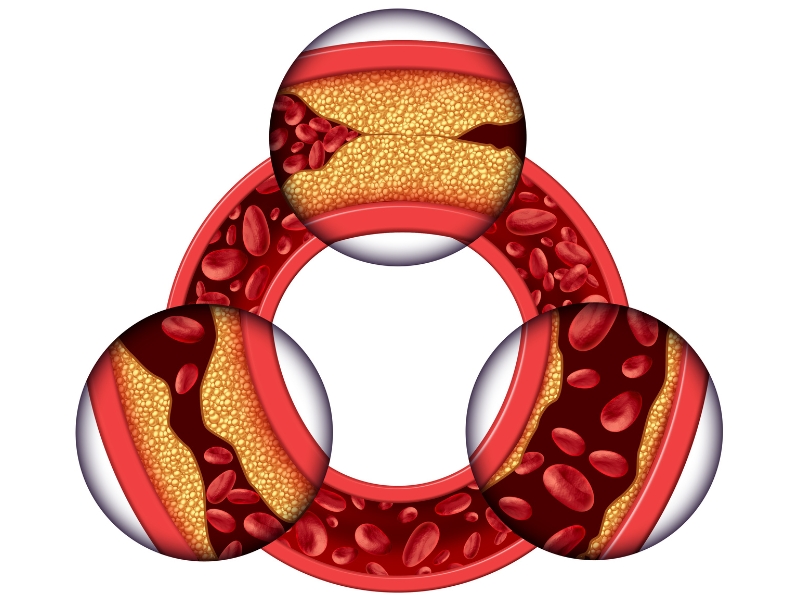
According to the Mayo Clinic, there are two primary causes of heart failure: coronary artery disease (blocked coronary arteries) and hypertension (high blood pressure). Atherosclerosis is a condition characterized by the building up of a plaque of fats and cholesterol and other substances on the inner walls of the coronary arteries, restricting blood flow and increasing the danger of a blood clot’s breaking free from the plaque and cutting off blood flow.
High blood pressure will cause the heart muscle to thicken over time, making the brief period of relaxation between heart beats more difficult, and making it more difficult for the heart to fill up adequately with blood to pump out to the organs.
Then, there are other causes such as the following:
- congenital heart disease
- heart attack
- leaky or narrowed heart valves
- infection or inflammation of the heart muscle
- abnormal heart rhythms (arrhythmia)
Functional categories of heart failure
The New York Heart Association classifies the degree of the severity of the heart failure according to the following four functional categories, from least severe to most severe:
I able to do ordinary physical activity without undue fatigue, pain, or shortness of breath
II able to feel comfortable at rest but, during ordinary physical activity, feeling some undue fatigue, heart palpitation, angina pain, or shortness of breath
III still able to feel comfortable at rest but, with less than ordinary physical activity, feeling fatigue, heart palpitation, angina pain, or shortness of breath
IV unable to carry out any type of physical activity without discomfort and having symptoms of heart failure even at rest
Dr. Svend Aage Mortensen on causes of heart failure
Dr. Mortensen, the lead researcher on the Q-symbio clinical trial and a cardiologist at the Heart Centre of the Copenhagen University Hospital, acknowledges that there are multiple causes of heart failure, which is difficult to treat, but he focuses in on the question of bio-energetics and the role that the availability/the non-availability of Q10 plays in what he calls energy starvation in the heart muscle cells.
Dr. Mortensen points out that adjunctive treatment with Q10 is intended to boost the production of energy in the heart muscle cells whereas the standard treatments for heart failure — ACE inhibitors, angiotensin II receptor blockers, beta-blockers, calcium channel blockers, diuretics, and vasodilators — are designed to block specific cellular processes.
The Q-symbio study shows that using Q10 to address the problem of dysfunctional energy production in the heart has the potential to help heart failure patients improve their New York Heart Association status and to avoid being re-admitted to the hospital. For many heart failure patients, that improvement in NYHA functional class will translate into more ability to move around and be active with less fatigue and less discomfort.
Q10 supplementation and coronary artery disease
Elsewhere in this q10facts.com blog, I have described the studies showing the efficacy of Q10 in the treatment of hypertension. And we have already seen in an article on this website that, based on the results of eight rigorous clinical trials, Dr. de Frutos and the cardiologists at the University of Navarra Clinic in Pamplona, Spain, recommend the use of a well-absorbed Q10 preparation as a prophylactic treatment to prevent complications in patients undergoing bypass surgery.
A quick search of the Medline database reveals that a team of Taiwanese doctors has carried out a couple of Q10 intervention trials with coronary artery disease patients who had a 50% or more abnormal narrowing of at least one coronary artery and who had been taken a cholesterol-lowering statin medication for at least one month prior to the beginning of the studies.
In a study published in 2013, researchers reported that 42 coronary artery disease patients had been randomly assigned to a placebo group or to a 300 mg Q10 (150 mg twice daily) group for a period of 12 weeks (1). The results of the study showed that, in the Q10 treatment group, there were statistically significant rises in the levels of the plasma Q10 and statistically significant rises in the activity of antioxidant enzymes such as superoxide dismutase, catalase, and glutathione peroxidase. At the same time, the researchers discovered statistically significantly lower levels of a bio-marker of inflammation (tumor necrosis factor-α) following the supplementation withQ10.
The Taiwanese researchers concluded that administering 300 mg of Q10 per day to coronary artery disease patients on statin medications will significantly promote antioxidant enzyme activity and will significantly lower inflammation levels.
In a study published in 2012, the same Taiwanese researchers reported on the results of a randomized clinical trial with a placebo group, a 60 mg per day Q10 treatment group, and a 150 mg per day Q10 treatment group (2). The individuals enrolled in the study were patients who had been found to have at least 50% abnormal narrowing of at least one major coronary artery and who had been prescribed a statin medication. The study was conducted over a 12-week period, and the patients’ blood samples were analyzed every 4 weeks for plasma Q10 levels, malondialdehyde levels, and antioxidant enzyme (catalase, superoxide dismutase, and glutathione peroxidase) levels.
The findings showed that supplementation with 150 mg per day of Q10 increased plasma concentrations of Q10 significantly, lowered malondialdehyde levels significantly, and increased the levels of catalase and superoxide dismutase significantly. Malondialdehyde is a bio-marker for oxidative stress, which is the harmful effect of reactive oxygen species on cell metabolism. The researchers concluded that daily supplementation with at least 150 mg of Coenzyme Q10 reduces the extent of oxidative stress and increases the activity of antioxidant enzymes in patients diagnosed with coronary artery disease.
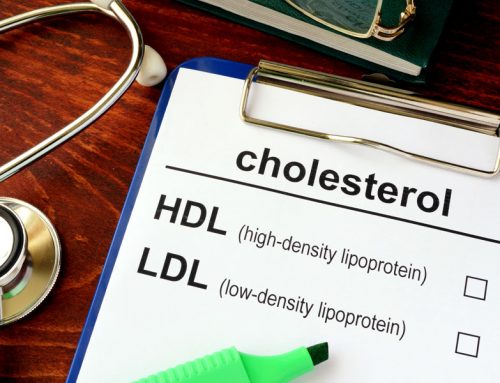
Q10 and statin medications
After I had read and digested the Taiwanese research reports, I realized that the really important reason for treating the coronary artery disease patients with Q10 supplements was that the patients were taking a statin medication. Yes, the statin medication was being used to lower the patients’ cholesterol levels by inhibiting the action of the HMG-CoA reductase enzyme. Unfortunately, inhibiting the action of this enzyme also shuts off the bio-synthesis of Q10, causing Q10 deficiency in the body; hence the vital need for Q10 supplementation in these Taiwanese patients.
An alternative theory proposed by Dr. Langsjoen
Then, not too long after I had read about the Taiwanese research, I happened to find a 2015 article by Dr. Peter Langsjoen, a cardiologist in Tyler, Texas, with long connections to Q10 research. Dr. Langsjoen suggests that, in addition to stifling the body’s own synthesis of Q10, statin medications could well be inhibiting the biosynthesis of vitamin K2 and the biosynthesis of important selenoproteins. According to Dr. Langsjoen’s conjecture — I emphasize that, at this stage, what Dr. Langsjoen writes is conjecture, not fact –, when we take statin medications, we may actually be aggravating the development of plaque in our arteries and we may be impairing the work of the heart muscle more than we are helping. Accordingly, Dr. Langsjoen urges that the treatment guidelines for the use of statin medications be re-evaluated. While we wait for this critical re-evaluation, let’s agree that we need to take a Q10 supplement and a selenium supplement if we are on statin medication.
Sources:
- Lee, B. Tseng, Y.F., Yen, C.H. & Lin, P. (2013). Effects of coenzyme Q10 supplementation (300 mg/day) on antioxidation and anti-inflammation in coronary artery disease patients during statins therapy: a randomized, placebo-controlled trial. Nutrition Journal, 12(1):142. doi: 10.1186/1475-2891-12-142.
- Lee B.J., Huang Y.C., Chen S.J., & Lin P.T. (2012). Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with coronary artery disease. Nutrition. 28(3):250-5. doi: 10.1016/j.nut.2011.06.004. Epub 2011 Oct 12







Leave A Comment