How to formulate supplementary Coenzyme Q10 so that CoQ10 molecules can cross the blood-brain barrier is an important research project. Why? Firstly, because CoQ10 is essential for cellular ATP energy generation. The brain is a big consumer of energy. Secondly, because more CoQ10 in the brain may be useful for the prevention and treatment of neurological disorders such as Alzheimer’s and Parkinson’s [Mantle 2025].
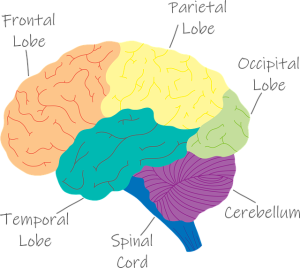
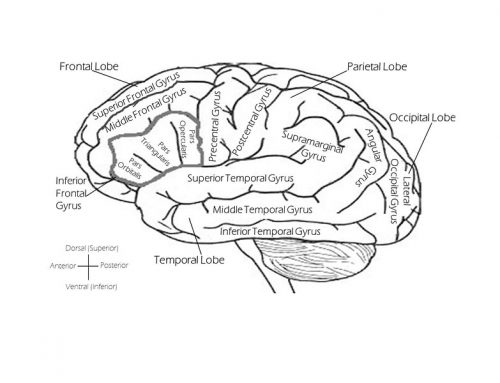
Cells lining blood vessels in the brain form a restrictive barrier. These cells are joined together very tightly. They permit the passage of essential substances and restrict the passage of harmful substances from the blood circulation to the brain cells.
CoQ10 is synthesized in nearly all types of human cells, including brain cells. Typically, human bio-synthesis of CoQ10 reaches its peak at age 25 years. After that, the extent of CoQ10 bio-synthesis declines with increasing age. The older one is, the less CoQ10 is produced in the brain and elsewhere. Most individuals above the age of 40 will benefit from a daily CoQ10 supplement.
In addition to being needed for ATP energy generation, CoQ10 acts as a fat-soluble antioxidant and an anti-inflammatory agent. As a nutritional supplement, CoQ10 protects against aging, cardiovascular disease, and low energy syndrome disorders [Alehagen 2022; Mortensen 2014; Mantle 2025].
CoQ10 and the Brain
With respect to CoQ10 and the brain, two points merit attention up front [Mantle 2025]:
1. Evidence that Coenzyme Q10 may cross the blood-brain barrier in laboratory animals to a small extent is not proof that Coenzyme Q10 will cross the blood-brain barrier in humans. The blood-brain barrier in animals seems to be considerably less restrictive than it is in humans [Mantle 2025].
2. Evidence that Coenzyme Q10 may cross the blood-cerebrospinal fluid barrier is not proof that Coenzyme Q10 will also cross the blood-brain barrier. Crossing the blood-brain barrier and crossing the cerebrospinal fluid are two entirely different mechanisms [Mantle 2025].
Compared to the blood-brain barrier, the blood-cerebrospinal fluid barrier is somewhat “leaky”. Accordingly, some limited but measurable access of CoQ10 into the cerebrospinal fluid does not mean that the same administration of CoQ10 will increase brain CoQ10 concentration. It would incorrect to suggest this [Mantle 2025].
Oral CoQ10 and the Blood-Brain Barrier

Researcher Iain P. Hargreaves and his team have observed brain CoQ10 influx and efflux in in-vitro and animal studies. There are no human studies showing orally administered CoQ10 associated with increased CoQ10 content in the brain. Cerebrospinal fluid CoQ10 levels are not appropriate proxies for brain CoQ10 levels.
The ability of orally administered CoQ10 to permeate the blood-brain barrier is very limited. Furthermore, to a certain extent, efflux mechanisms pump CoQ10 that has crossed the blood-brain barrier back into the blood circulation [Hargreaves 2025; Wainwright 2020]. Similarly, orally administered CoQ10 permeates the cerebrospinal fluid barrier only to a very limited degree [Mantle 2025].
Mantle et al suggest two possible ways for substances to cross the blood-brain barrier: passive diffusion and carrier/receptor-mediated transport.
- CoQ10 molecules seem to be too large to cross the blood-brain barrier via diffusion.
- To date, there are no studies identifying carriers/receptors for CoQ10 in the human brain cells, neither for the ubiquinol form nor for the ubiquinone form of CoQ10.
- At this writing, no clinical studies show that orally administered CoQ10 is associated with increases in brain tissue CoQ10 concentrations.
- Mantle et al are dubious about the use of CoQ10 analogues such as mitoquinone and idebenone to access the mitochondria in brain cells. The CoQ10 analogue products differ from CoQ10 in various aspects of intracellular function.
CoQ10 and Mitochondrial Dysfunction
Mitochondrial dysfunction is a condition in which the mitochondria – the cells’ powerhouses – fail to generate sufficient chemical energy. This dysfunction can have serious implications for organs that need high quantities of energy, e.g., the brain and the heart [Mantle 2025].
Mitochondrial dysfunction is a factor in the development of neurological disorders, i.e., Parkinson’s disease, Alzheimer’s disease, amyotrophic lateral sclerosis, and multiple system atrophy. Mantle et al cite evidence for a deficiency of CoQ10 in these neurological disorders [2025].
CoQ10 promotes normal mitochondrial function. CoQ10 protects the mitochondria against oxidative damage. Consequently, there is good reason to investigate the therapeutic role of CoQ10 supplementation [Mantle 2025].
Intranasal Administration of CoQ10
One possible way to deliver CoQ10 to human brain cells and tissues might be the formulation of a CoQ10 spray for intranasal administration. To date, however, there have been no clinical studies testing the safety and efficacy of intranasal delivery of CoQ10 to the brain [Mantle 2025].
Conclusion: CoQ10 Supplementation and Brain CoQ10 Concentrations
Beware of claims that any specific form or formulation of supplementary CoQ10 will increase the CoQ10 content in brain cells and tissues.
Beware of claims that the ubiquinol form of CoQ10 supplement has better absorption and bioavailability than the ubiquinone form.
Know that CoQ10 absorption and bioavailability depend much more on the formulation of the supplement than on the form of the supplement.
Whether CoQ10 supplement uses ubiquinol or ubiquinone is less important than the manufacturer’s choice of carrier oils and heating and cooling processes.
Sources
Alehagen U et al. Improved cardiovascular health by supplementation with selenium and coenzyme Q10: applying structural equation modelling (SEM) to clinical outcomes and biomarkers to explore underlying mechanisms in a prospective randomized double-blind placebo-controlled intervention project in Sweden. Eur J Nutr. 2022 Sep;61(6):3135-3148.
Hargreaves IP. The Utility of Coenzyme Q10 in the treatment of neuronal mitochondrial dysfunction. Conference presentation, 19 June 2025. Copenhagen: 11th Conference of the International Coenzyme Q10 Association.
Mantle D, Hargreaves I. Coenzyme Q10 and the blood-brain barrier: an overview. J Clin Med. 2025 Apr 16;14(8):2748.
Mortensen SA et al. The effect of Coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-Symbio: a randomized double-blind trial. JACC Heart Fail. 2014 Dec;2(6):641-9.
Wainwright L et al. CoQ10 deficient endothelial cell culture model for the investigation of CoQ10 blood-brain barrier transport. J. Clin. Med. 2020;9:3236.
The information presented in this review article is not intended as medical advice. It should not be used as such.





Leave A Comment