Coenzyme Q10 is a vitamin-like substance that is found in all human tissues, with the highest concentrations in the heart, brain, kidney, and liver.
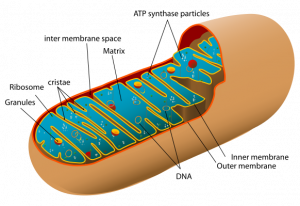
The mitochondria (singular: mitochondrion) in our cells are known as the “powerhouses of the cell.” Mitochondria produce the energy needed for the functioning of the cells. Basically, they do this via chemical reactions that convert glucose to ATP energy molecules. Coenzyme Q10 is essential to this process.
Coenzyme Q10 supports mitochondrial function in the cells through its essential role in the generation of ATP energy. It is also a powerful lipid-soluble antioxidant, protecting the cells against damage caused by harmful free radicals [Xu 2022].
Unfortunately, in middle age and in the senior years, the cellular bio-synthesis of Coenzyme Q10 declines with increasing age [Kalen 1989]. One estimate suggests that the bio-synthesis of Coenzyme Q10 in heart muscle cells is reduced to half at 80 years [Alehagen 2021]. It is practically impossible to replace the lost endogenous Coenzyme Q10 by improving dietary intakes: there is a definite need for daily supplementation with a bio-available CoQ10 supplement [Mantle & Dybring 2020].
Coenzyme Q10 and Neurodegenerative Disorders
Mitochondrial dysfunction – defined as a reduced capacity for the cellular generation of ATP energy and increased vulnerability to oxidative damage caused by harmful free radicals – plays a role in the development of a number of neurodegenerative disorders, including Parkinson’s disease, Alzheimer’s disease, amyotrophic lateral sclerosis, multi-system atrophy, and progressive supranuclear palsy [Mantle & Hargreaves 2022].
Coenzyme Q10 and Alzheimer’s Disease
A case-control study of approximately 6000 Japanese citizens aged 40-69 years at baseline has shown that low serum CoQ10 concentrations were inversely linked to the risk of developing dementia. There was a similar association between low CoQ10/total cholesterol ratio and the risk of dementia [Yamagishi 2014].
As of late 2022, no large clinical studies have assessed the effect of CoQ10 supplementation on cognitive decline and dementia [Mantle & Hargreaves 2022].
Coenzyme Q10 and Parkinson’s Disease
Various studies show reduced concentrations of Coenzyme Q10 in the cerebral cortex and in the plasma and platelets in patients with Parkinson’s disease [Mantle & Hargreaves 2020].
Studies of CoQ10 supplementation have shown contradictory results:
- A 2002 clinical trial using oral CoQ10 supplementation (300–1200 mg/day) showed a reduction in the functional decline of patients with early-stage Parkinson’s disease [Shults 2002].
- A 2014 clinical trial using CoQ10 dosages of 1200 or 2400 mg/day appeared to show no apparent clinical benefit [Beal 2014].
- The contradictory outcomes of the two studies may be a result of the broad heterogeneity of patients enrolled in the two clinical trials [Mantle & Hargreaves 2022].
Coenzyme Q10 and amyotrophic lateral sclerosis
In the only randomized controlled test reported to date, a phase II test of CoQ10 supplementation of 185 amyotrophic lateral sclerosis patients at 2,700 mg daily for nine months showed insufficient promise to warrant Phase III testing.
Note: Phase II tests are designed to test efficacy of an experimental drug on a particular disease or condition in 100 to 300 volunteers over a period of several months to two years.
Phase III tests are designed to test the safety and efficacy of an experimental drug at multiple centers with several hundred to several thousand patients.
Coenzyme Q10 and Multiple System Atrophy
Clinical studies have shown reduced CoQ10 concentrations in the plasma and in the postmortem brain tissue of patients with multiple systems atrophy [Mantle & Hargreaves 2022].
As of late 2022, there have been no reports of randomized controlled trials of CoQ10 supplementation of patients with multiple systems atrophy [Mantle & Hargreaves 2022].
Conclusion: Coenzyme Q10 and Neurodegenerative Disorders
The current state of the research literature is unsatisfactory. Despite evidence that reduced blood and tissue concentrations of Coenzyme Q10 are common in patients with neurodegenerative disorders, there have been very few randomized controlled trials of the effect of CoQ10 supplementation on these patients. The few clinical trials that have been conducted have given contradictory results [Mantle & Hargreaves 2022].
The hitherto lack of efficacy of Coenzyme Q10 in the treatment of neurodegenerative diseases may reflect the need for a formulation and a form of administration that enables the supplemented Coenzyme Q10 to cross the blood–brain barrier [Mantle & Hargreaves 2022].
Moreover, it may be that the administration of Coenzyme Q10 to patients with neurodegenerative disorders would be more effective in combination with other micronutrients such as selenium or carnitine. There is, for example, research evidence of a synergistic interaction between Coenzyme Q10 and selenium [Alehagen & Aaseth 2015].
The best estimate for a therapeutic effect of Coenzyme Q10 on neurodegenerative diseases is that the supplementation would need to increase plasma/serum CoQ10 concentrations to 3.5 mg/L [Langsjoen 2014, p. 16].
Sources
Alehagen U, Johansson P, Svensson E, Aaseth J, Alexander J. Improved cardiovascular health by supplementation with selenium and coenzyme Q10: applying structural equation modelling (SEM) to clinical outcomes and biomarkers to explore underlying mechanisms in a prospective randomized double-blind placebo-controlled intervention project in Sweden. Eur J Nutr. 2022 Sep;61(6):3135-3148.
Alehagen U, Aaseth J. Selenium and coenzyme Q10 interrelationship in cardiovascular diseases–A clinician’s point of view. J Trace Elem Med Biol. 2015;31:157-62.
Beal MF, Oakes D, Shoulson I, Henchcliffe C, Galpern WR, Haas R, Juncos JL, Nutt JG, Voss TS, Ravina B. A randomized clinical trial of high-dosage coenzyme Q10 in early Parkinson disease: No evidence of benefit. JAMA Neurol. 2014;71:543–552.
Kalen A, Appelkvist EL, Dallner G (1989) Age-related changes in the lipid compositions of rat and human tissues. Lipids. 24:579–584.
Langsjoen PH, Langsjoen AM. Comparison study of plasma coenzyme Q10 levels in healthy subjects supplemented with ubiquinol versus ubiquinone. Clin Pharmacol Drug Dev. 2014 Jan;3(1):13-7.
Mantle D, Dybring A. Bioavailability of Coenzyme Q10: An overview of the absorption process and subsequent metabolism. Antioxidants (Basel). 2020 May 5;9(5):386.
Mantle D, Hargreaves IP. Mitochondrial dysfunction and neurodegenerative disorders: role of nutritional supplementation. Int J Mol Sci. 2022 Oct 20;23(20):12603.
Shults CW, Oakes D, Kieburtz K, Beal MF, Haas R, Plumb S, Juncos JL, Nutt J, Shoulson I, Carter J. Effects of coenzyme Q10 in early Parkinson disease: Evidence of slowing of the functional decline. Arch. Neurol. 2002; 59:1541–1550.
Xu J, Jin X, Ye Z, Wang D, Zhao H, Tong Z. Opposite roles of Co-enzyme Q10 and formaldehyde in neurodegenerative diseases. Am J Alzheimers Dis Other Demen. 2022 Jan-Dec;37:15333175221143274.
Yamagishi K, Ikeda A, Moriyama Y, Chei CL, Noda H, Umesawa M, Cui R, Nagao M, Kitamura A, Yamamoto Y, Asada T, Iso H; CIRCS Investigators. Serum coenzyme Q10 and risk of disabling dementia: the Circulatory Risk in Communities Study (CIRCS). Atherosclerosis. 2014 Dec;237(2):400-3.
The information presented in this review article is not intended as medical advice and should not be used as such.
15 January 2023



Leave A Comment