
Mitochondrial dysfunction, oxidative stress, and inflammation have been implicated in the development of non-alcoholic fatty liver disease (NAFLD). Treatment with the essential bio-nutrient Coenzyme Q10 may improve the prognosis for NAFLD patients. CoQ10 has a key role in mitochondrial function as well as having antioxidant and anti-inflammatory action. CoQ10 levels are depleted in NAFLD.
The results of two randomized controlled studies indicate that CoQ10 supplement at a dosage of 100 mg/day can be effective in reducing systemic inflammation and in improving biochemical variables associated with Non-Alcoholic Fatty Liver Disease (NAFLD) [Farsi 2016; Farhangi 2014].
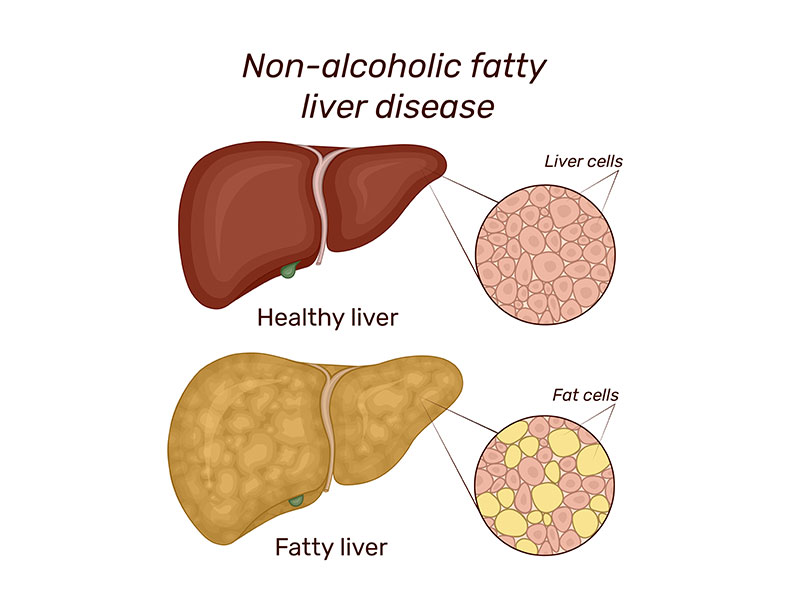
NAFLD is a chronic liver disorder related to systemic inflammation.
- The NAFLD condition exists whenever the accumulation of fat in the liver cells, primarily in the form of triglycerides, exceeds 5–10% of liver weight.
- NAFLD is the most common liver disorder worldwide; its prevalence in the general population is estimated at 20–30%.
- NAFLD’s prevalence increases to 60–70% in obese individuals and to 70–90% in individuals with diabetes [Mantle & Hargreaves 2020].
Coenzyme Q10 is an essential bio-nutrient that has been shown to reduce the blood levels of bio-markers of systemic inflammation [Fan 2017; Zhai 2017]. Moreover, number of pre-clinical studies have demonstrated the capacity of supplemental Coenzyme Q10 to prevent or reduce the extent of liver tissue damage by a variety of toxic agents [Mantle & Hargreaves 2020].
Consequently, it is logical to test the anti-inflammatory properties of CoQ10 supplements in NAFLD patients [Farsi 2016].
CoQ10 Supplementation of NAFLD Patients
In a 2016 study, researchers assigned 41 NAFLD patients randomly to a CoQ10 treatment group (100 mg/day) or a placebo group. The study duration was 12 weeks, long enough to see an effect of the CoQ10 supplementation. Blood samples were taken from each patient at the start of the study and at the end of the study [Farsi 2016].
Taking the Coenzyme Q10 daily was associated with the following beneficial effects compared to the placebo treatment [Farsi 2016]:
- significant reductions in the levels of liver aminotransferases (aspartate aminotransferase and gamma-glutamyl transpeptidase)
- significant reductions in the levels of bio-markers for systemic inflammation (high-sensitivity C-reactive protein and tumor necrosis factor alpha)
- significant reductions in the grades of NAFLD
In a 2014 study, researchers randomly assign 44 NAFLD patients to take Coenzyme Q10 100 mg/day or placebo for four weeks. The study results showed that CoQ10 supplementation is associated with a significant reduction in blood levels of a liver enzyme (aspartate aminotransferase).
When liver cells are damaged, they release higher levels of aspartate aminotransferase. The study data also showed an association between CoQ10 supplementation and a significant reduction in the blood levels of bio-markers for oxidative stress [Farhangi 2014].
Coenzyme Q10 and Liver Disease
Dr. David Mantle makes the following connections between CoQ10 status and liver disease, both non-alcohol related and alcohol related liver disease [Mantle & Hargreaves 2019].
- The liver is a major site of CoQ10 bio-synthesis.
- A reduction of CoQ10 bio-synthesis is likely in patients with reduced metabolic capacity in the liver.
- NAFLD is a known risk factor for cardiovascular disease.
- NAFLD is associated with heart failure, arrhythmias, valve dysfunction, and atherosclerosis.
- Alcohol-related liver disease is also associated with an increased risk of cardiovascular disorders; in particular alcoholic cardiomyopathy, arterial hypertension, and atrial fibrillation.
- Reduced CoQ10 bio-synthesis will be a problem in NAFLD patients prescribed statins; statin medications inhibit not only the bio-synthesis of cholesterol but also the bio-synthesis of Coenzyme Q10.
Dr. Mantle explains that CoQ10 supplementation should benefit NAFLD patients by reducing the levels of systemic inflammation and by reducing the oxidative damage caused by harmful free radicals. In its reduced form (called ubiquinol), Coenzyme Q10 functions as an important fat-soluble antioxidant [Mantle & Hargreaves 2019].
In his 2018 book, The Insider’s Guide to Coenzyme Q10, now available from amazon.com, Dr. William Judy summarizes and discusses the clinical benefits of CoQ10 supplementation.
Bottom line: Coenzyme Q10 Supplementation
Coenzyme Q10 supplementation is necessary even for healthy people as they get older. Once people reach adulthood, their cells produce less Coenzyme Q10 with increasing age [Kalen 1989].
CoQ10 supplementation has many beneficial health effects:
- improves symptoms and survival in heart failure patients [Mortensen 2014]
- improves heart function and survival in senior citizens [Alehagen 2013]
- improves physical function in patients with Gulf War Illness [Golomb 2014]
- improves symptoms in patients with statin-induced myopathy [Fedacko 2013]
- improves follicular fluid oxidative metabolism and oocyte quality, specially in over 35-year-old women [Giannubilo 2018]
There is much variability in the forms and formulations of CoQ10 supplements [Lopez-Lluch 2019]. It is important to buy a CoQ10 supplement with documented absorption and efficacy.
References
Alehagen U, Johansson P, Björnstedt M, Rosén A, & Dahlström, U. (2013). Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and Coenzyme Q10 supplementation: a 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. International Journal of Cardiology, 167(5), 1860-1866.
Fan L, Feng Y, Chen GC, Qin LQ, Fu C, & Chen LH. (2017). Effects of coenzyme Q10 supplementation on inflammatory markers: A systematic review and meta-analysis of randomized controlled trials. Pharmacological Research, 119, 128–136.
Farhangi MA, Alipour B, Jafarvand E & Khoshbaten M. (2014). Oral CoQ10 supplementation in patients with NAFLD: Effects on serum vaspin, chemerin, pentraxin, insulin resistance and oxidative stress. Arch. Med. Res.; 45:589–595.
Farsi F, Mohammadshahi M, Alavinejad P & Rezazadeh A. (2016). Functions of Coenzyme Q10 supplementation on liver enzymes, markers of systemic inflammation, and adipokines in patients affected by nonalcoholic fatty liver disease. J Am Coll Nutr; 35: 346-53.
Fedacko J & Pella D. (2013). Coenzyme Q(10) and selenium in statin-associated myopathy treatment. Can J Physiol Pharmacol; 91: 165-70.
Giannubilo SR, Orlando P, Silvestri S, Cirilli I, et al. (2018). CoQ10 supplementation in patients undergoing IVF-ET: The relationship with follicular fluid content and oocyte maturity.; Antioxidants (Basel); 10: 141.
Golomb, B. (2014). CoQ10 and Gulf War illness. Neural Computation; 26 (11): 2594-651.
Kalén A, Appelkvist EL & Dallner G. (1989). Age-related changes in the lipid compositions of rat and human tissues. Lipids, 24(7):579–584.
López-Lluch G, Del Pozo-Cruz J, Sánchez-Cuesta A, Cortés-Rodríguez AB, & Navas P. (2019). Bioavailability of coenzyme Q10 supplements depends on carrier lipids and solubilization. Nutrition, 57, 133–140.
Mantle D & Hargreaves I. (2019). Coenzyme Q10 and degenerative disorders affecting longevity: an overview. Antioxidants (Basel); 8(2): E44.
Mantle D & Hargreaves I. (2020). Coenzyme Q10 supplementation in non-alcoholic fatty liver disease: an overview. Liver Nursing Supplement; S1-S7.
Mortensen SA, Rosenfeldt F, Kumar A, Dolliner P, Filipiak KJ, Pella D & Littarru GP. (2014). The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC. Heart Failure, 2(6), 641-649.
Zhai J, Bo Y, Lu Y, Liu C & Zhang L. (2017). Effects of Coenzyme Q10 on markers of inflammation: a systematic review and meta-analysis. Plos One, 12(1), e0170172.
The information presented in this review article is not intended as medical advice and should not be construed as such.
16 March 2020



Leave A Comment