The blood-brain barrier. For a number of years, CoQ10 researchers have discussed whether Coenzyme Q10 from the diet and from supplements is able to cross the blood-brain barrier. Now, using a cell culture model, the CoQ10 researchers Iain Hargreaves from John Moore’s University in Liverpool and Jane Preston and Luke Wainwright from University College Hospitals in London have brought a bit of clarity to this debate. In May, 2022, Hargreaves presented their research at an international Coenzyme Q10 conference in Hamburg, Germany.
The Blood-Brain Barrier: Multiple Layers of Cells
First, it is useful to know a little about the blood-brain barrier (BBB). The BBB is not a physical membrane that lines the brain but consists, rather, of the multiple layers of semi-impermeable cells in the blood vessels (capillaries) that surround the brain. Inside these blood vessels are the endothelial cells, which make up the cell walls of the blood vessels and which carry out the actual barrier function. The endothelial cells in the BBB differ from endothelial cells in the blood vessels elsewhere in the body by being very tightly packed.
The protein structures between the endothelial cells in the blood vessels in the brain are tight junctions that prevent the uncontrolled passage of substances between the endothelial cells. On the outside of the endothelial cells, there is a basement membrane, in which there is a layer of pericytes that work together with the endothelial cells and that have a stabilizing function on the blood vessels in the brain. The pericytes register which substances are present in the blood and decide whether these substances may pass BBB or not.
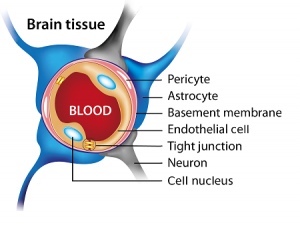
Figure 1. Illustration of the blood brain barrier. In Figure 2 below, there is an illustration of the endothelial cells of the blood-brain barrier with their different transport proteins and with tight junctions between the cells.
For further protection in the event of infections, white blood cells of the macrophage type can cross the blood-brain barrier and swallow unwanted substances; however, these macrophages can also cause tissue damage. Moreover, there is the outermost layer of the basement membrane, which is made up of supporting cells called astrocytes. The astrocytes are responsible for the overall control over which substances are allowed to pass as well responsible for the maintenance of the BBB.
The Purpose of the Blood-Brain Barrier
Together, the cells in the BBB allow only certain substances to pass from the blood into the brain tissue and from the brain into the blood circulation.
The purpose of BBB is to maintain a constant chemical environment in the brain so that the brain cells get optimal safe conditions. It is primarily water-soluble substances that have difficulty passing the BBB whereas fat-soluble substances are able to pass more easily.
Here, one would think that Coenzyme Q10, which is fat-soluble, should pass easily, but research has shown that Coenzyme Q10 has difficulty in passing through the BBB. Normally, the BBB permits only water, oxygen, and small fat-soluble substances to pass through. The problem with Coenzyme Q10 molecules is that they are fairly large.
It is well established that deficiency of Coenzyme Q10 in the body tissues can be remedied after some time with supplementation of properly formulated CoQ10 supplements. It has therefore puzzled researchers that supplements with Coenzyme Q10 have provided only transient improvement in neurological symptoms, prompting debate as to whether exogenous Coenzyme Q10 is able to cross the blood-brain barrier.
Coenzyme Q10 and Blood-Brain Barrier Cell Study
To clarify this question, Hargreaves, Preston, and Wainwright used in-vitro models of the blood-brain barrier. These models consisted of cells from mouse brain and pig brain, in which the researchers could observe whether the supply of Coenzyme Q10 could pass under normal conditions and under conditions of CoQ10 deficiency in the brain tissue.
In the first phase of the study, Hargreaves, Preston, and Wainwright showed that, in normal conditions, the amount of Coenzyme Q10 crossing the blood-brain barrier from the blood side is matched by the efflux of Coenzyme Q10 being transported out of the blood-brain barrier and back into the blood. Therefore, overall, there seems to be no net uptake of Coenzyme Q10 into the brain under normal conditions, i.e., whenever the concentration of Coenzyme Q10 in the brain tissue is in the normal range.
Coenzyme Q10 inhibitor PABA
In the next phase of the experiment, Hargreaves, Preston, and Wainwright added the substance para-aminobenzoate (PABA) to the brain tissue. PABA has among its properties the inhibition of an enzyme necessary for the body’s cells to form Coenzyme Q10. After five days of PABA supplementation, the activity of mitochondrial enzyme complexes was reduced by 70%, and the brain tissue’s content of Coenzyme Q10 was reduced by 50%.
CoQ10 shortage allows net transfer
The PABA-induced considerable lack of Coenzyme Q10 in the brain tissue resulted in a net transfer of Coenzyme Q10 to the brain tissue. There was a greater amount of Coenzyme Q10 accessing the brain tissue than there was flowing out of the brain tissue. To understand this mechanism, it is helpful to look at the receptors in the endothelial cells and their tight junctions.
Transporters through the blood-brain barrier
Hargreaves lists a number of transporters on the surface of the endothelial cells, which have different purposes.
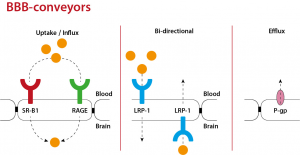
Figure 2. An illustration of the endothelial cells of the blood-brain barrier with their different transport proteins and with tight junctions between the cells. Attribution: Iain Hargreaves, 2022.
Hargreaves’ presentation in summary form
In their cell culture model, Hargreaves, Preston, and Wainwright tested factors that may be able to promote or inhibit the passage of the lipoproteins that would be expected to transport Coenzyme Q10 in the blood through the BBB. Lipoprotein transport across the BBB would be crucial for the delivery of Coenzyme Q10 (as well as other lipids) to the brain cells.
The researchers found that the RAGE receptor is important for the transport (influx) of Coenzyme Q10 from the blood into the brain, and that the LRP-1 transporter is important for the transport (efflux) of Coenzyme Q10 from the brain to the blood. Furthermore, their experiments showed that the SRB1 transporter does not play an important role in the transfer of Coenzyme Q10 into or out of the brain.
- LRP-1 (LDL-related protein 1) is a carrier for the efflux of Coenzyme Q10 from the brain. Hargreaves suggested that an inhibition of LRP-1 could be beneficial in slowing the outflow of Coenzyme Q10 from the brain.
- An increase in RAGE was associated with a decreased density of BBB (more open tight junctions) and with increased transport of Coenzyme Q10 into the brain tissue.
If there is resistance to the transfer of Coenzyme Q10 from the blood to the brain, then the explanation may be 1) that the CoQ10 treatment has been started too late or 2) that there are poor transfer conditions.
Researchers in the audience at the international Coenzyme Q10 conference suggested that oral CoQ10 supplements may also help the brain in the following ways:
- By reducing the number of inflammatory proteins that cross into the brain
- By improving the quantity and quality of the mitochondria in the blood that cross into the brain
- By improving the endothelial function in the blood vessels and thereby improving the blood pressure and clotting factors in the blood
Conclusion
Under normal conditions in which the concentration of Coenzyme Q10 in the brain tissue is within a normal range, the blood-brain barrier does allow the passage of some Coenzyme Q10; however, the amount of Coenzyme Q10 permitted to access the brain is offset by the amount of Coenzyme Q10 exiting the brain, so there is no net gain of Coenzyme Q10 in the brain in normal circumstances.
In cases of a marked deficiency of Coenzyme Q10 in the brain, receptors on the endothelial cells allow the passage of Coenzyme Q10 into the brain in greater quantities than flow out of the brain, thus resulting in a net increase of Coenzyme Q10 in the brain tissue.
This model suggests that therapeutic supplements of Coenzyme Q10 to the brain may be transient in their effect. When the level of Coenzyme Q10 in the brain reaches the normal range, CoQ10 supplementation is unlikely to result in further increases in CoQ10 concentrations in the brain.
Sources
Hargreaves, IP. Can Coenzyme Q10 Cross the Blood-Brain Barrier? 2022, May 14. Conference presentation. 10th Conference of the International Coenzyme Q10 Association. Hamburg, Germany.
Mantle D, Heaton RA, Hargreaves IP. Coenzyme Q10, Ageing and the Nervous System: An Overview. Antioxidants (Basel). 2021 Dec 21;11(1):2.
Wainwright, Luke. Mechanisms of Coenzyme Q10 Blood-Brain Barrier Transport. 2018. Doctoral thesis (Ph.D), UCL (University College London).
The information presented in this review article is not intended as medical advice and should not be used as such.
15 August 2022








Leave A Comment